Magnesium and Blood Sugar Control: How This Essential Mineral Can Transform Diabetes Care
July 31, 2023
 678
678 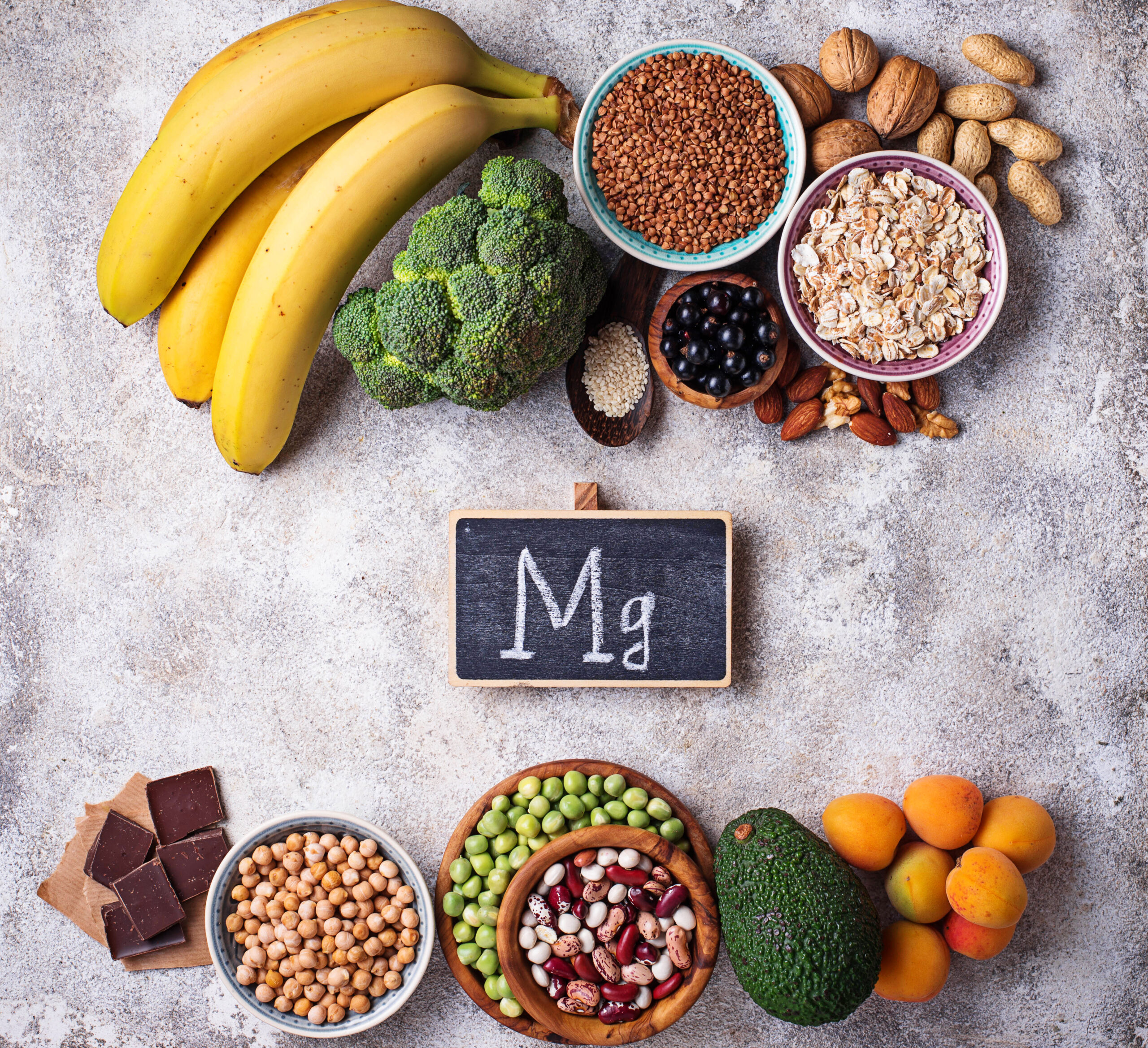
Type 2 diabetes is a chronic condition characterized by the body’s inability to effectively use insulin, leading to elevated blood sugar levels.
It is a global health concern, affecting over 400 million people worldwide, and its prevalence continues to rise, particularly in developing countries.
This condition can lead to severe complications such as heart disease, kidney failure, and blindness if not properly managed.
Enter magnesium—a vital mineral that plays a central role in over 300 biochemical functions in the human body, ranging from energy production to bone health.
Yet, its significance does not end there.
Recent studies have begun to uncover a fascinating relationship between magnesium and diabetes, hinting at its potential role in the management and even prevention of this debilitating disease.
In this blog, we’ll delve into the science behind magnesium’s influence on glycemic control and insulin sensitivity, shedding light on how this essential mineral can be a vital tool in the fight against type 2 diabetes.


Magnesium is more than a simple element on the periodic table.
Within the human body, it acts as a co-factor in numerous enzymatic reactions that control everything from muscle contraction to nerve function.
It is crucial in the production of ATP, the energy currency of the cell, making it indispensable for daily bodily functions.
But magnesium’s role extends further, particularly in the context of insulin sensitivity.
Insulin is a hormone that helps regulate blood sugar levels, and magnesium aids in this process by enhancing the effectiveness of insulin, thus helping to maintain normal glucose levels.
However, not everyone gets enough of this crucial mineral.
Magnesium deficiency is surprisingly common and can manifest in symptoms such as muscle cramps, fatigue, and irritability.
Even more concerning is the fact that individuals with type 2 diabetes often exhibit lower levels of magnesium in their blood.
Studies, such as the one published in the Journal of Human Nutrition and Dietetics in 2017, have shown a significant prevalence of magnesium deficiency in diabetic patients, leading to worse glycemic control.
This finding underscores the importance of magnesium not only in general health but specifically in the context of type 2 diabetes.
Understanding magnesium’s multifaceted role and the consequences of its deficiency opens new avenues in our approach to managing and possibly preventing type 2 diabetes.
It sets the stage for a closer examination of how diet, supplementation, and lifestyle changes can harness the power of this essential mineral for better health outcomes.
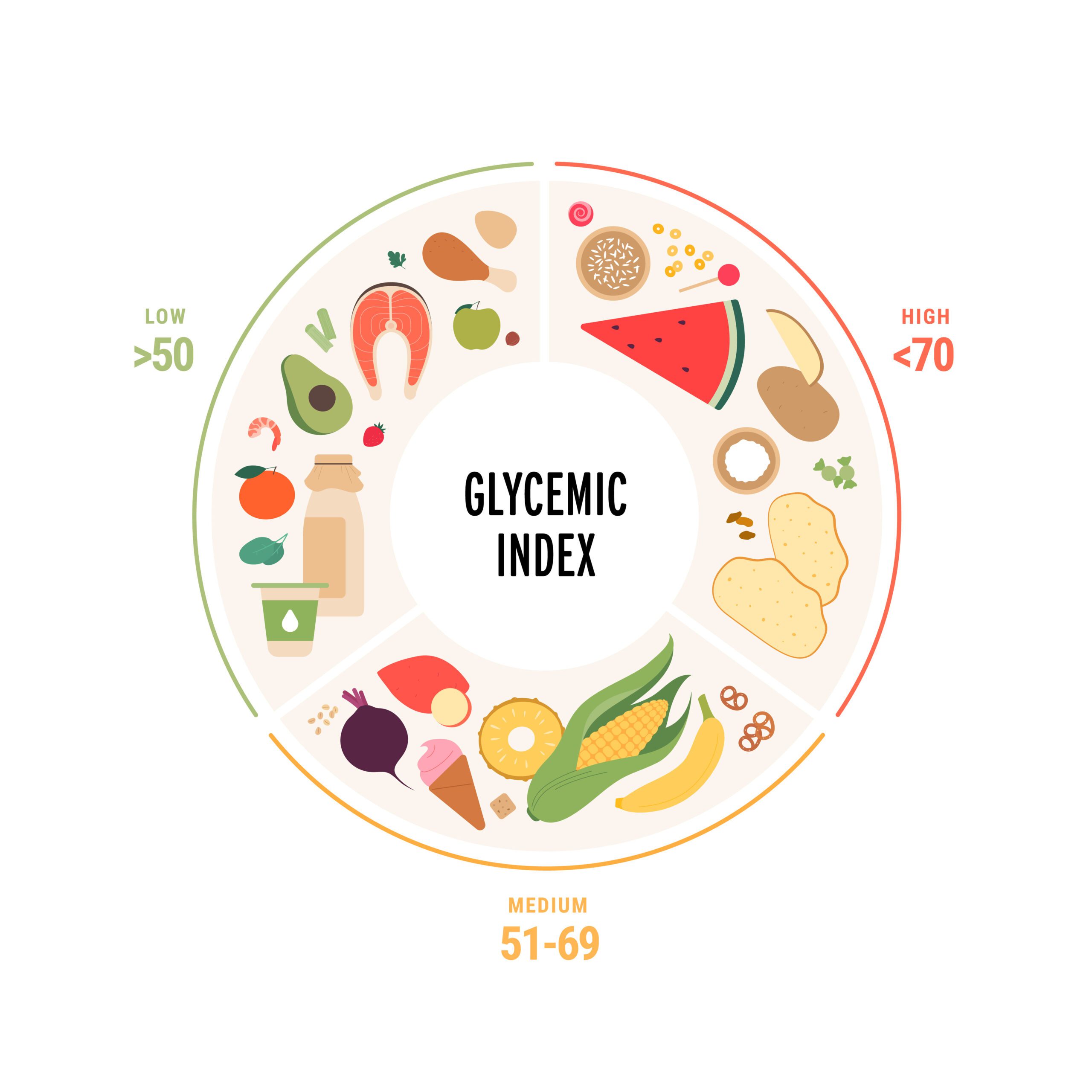
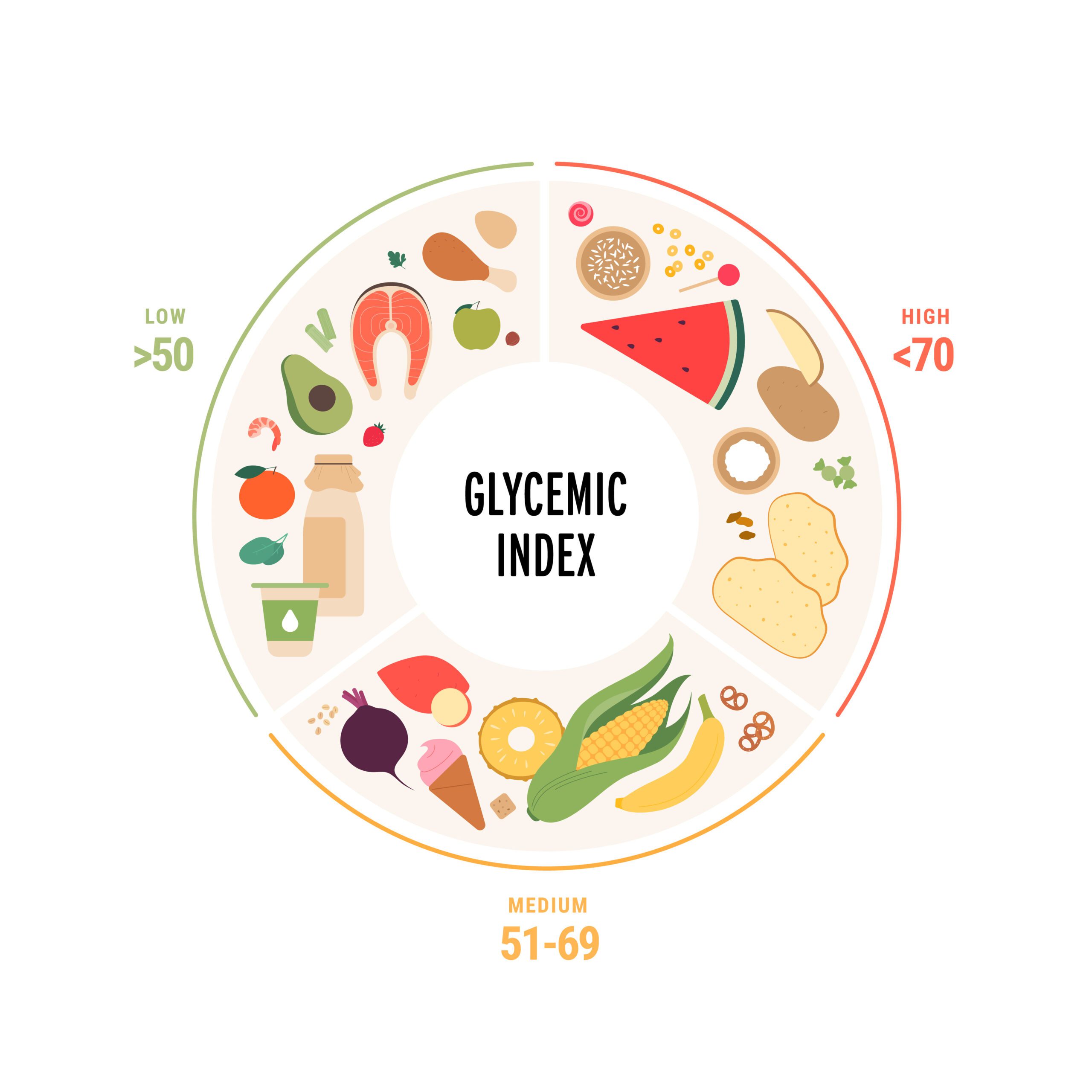
Blood sugar regulation is a complex but vital process for human health, and magnesium plays an integral role in it.
Its impact on glycemic control is multifaceted and deeply interconnected with insulin’s function, the hormone that allows glucose to enter cells and be used for energy.
Magnesium acts as a cofactor for several enzymes involved in glucose metabolism. Its presence helps to facilitate the precise reactions required to process glucose effectively.
Additionally, magnesium is known to enhance insulin sensitivity, meaning that the body needs less insulin to achieve the same blood sugar-lowering effect.
This process assists the cells in responding better to insulin, aiding in the efficient uptake of glucose from the blood.
Research underscores these mechanisms.
A meta-analysis published in the journal “Diabetes Care” in 2011 found that increased magnesium intake was associated with a reduced risk of developing type 2 diabetes.
Moreover, a 2014 study in the “European Journal of Clinical Nutrition” observed improved insulin sensitivity in type 2 diabetic patients following magnesium supplementation.
However, like any nutritional approach, magnesium’s role in glycemic control is not without potential risks or limitations.
Some individuals may experience side effects from excessive magnesium supplementation, such as diarrhea or abdominal cramping.
Moreover, the balance of magnesium with other minerals such as calcium needs careful consideration, as disproportionate levels might lead to other health issues.


The evidence linking magnesium intake with type 2 diabetes risk reduction and better management is indeed compelling, paving the way for practical applications in diabetes care.
Whether through diet or supplements, increasing magnesium levels can become an integral part of an individual’s diabetes management plan.
Dietary sources of magnesium are often the preferred approach.
Foods rich in magnesium include leafy green vegetables, whole grains, nuts, and seeds.
Incorporating these into a balanced diet not only promotes overall health but also provides a natural way to boost magnesium levels.
However, dietary changes might not be enough for everyone.
In such cases, magnesium supplements can be an effective alternative.
A 2017 study published in “Diabetes & Metabolism” demonstrated that magnesium supplementation could significantly improve insulin resistance in diabetic patients, especially those with a magnesium deficiency.
But one size does not fit all when it comes to supplementation.
Individual variations, such as age, existing health conditions, and the severity of magnesium deficiency, must be taken into account.
Consultation with healthcare professionals, such as dietitians or endocrinologists, is essential to determine the most suitable approach tailored to each person’s needs.
In conclusion, both dietary adjustments and supplementation present viable ways to harness magnesium’s potential in type 2 diabetes management.
Through evidence-based practices, these strategies can be customized to meet the unique needs and preferences of each individual, contributing to more effective prevention and treatment of this widespread condition.


Clinical trials and real-world evidence have cemented magnesium’s role in managing type 2 diabetes.
Several longitudinal studies, such as the 15-year study conducted by the Harvard School of Public Health, have identified an inverse relationship between magnesium intake and the risk of type 2 diabetes.
Furthermore, clinical trials like the one published in “Diabetes, Obesity and Metabolism” in 2016 have demonstrated that magnesium supplementation leads to improvements in blood glucose levels and insulin function in diabetic patients.
Patient testimonials also underscore the effectiveness of magnesium interventions.
Many individuals have reported an improvement in their blood sugar control and overall well-being after incorporating magnesium-rich foods or supplements into their regimen.
These firsthand experiences add personal insights to the scientific understanding of magnesium’s role.
Current guidelines from reputable health organizations, such as the American Diabetes Association, are beginning to recognize the importance of magnesium.
While it’s not yet considered a frontline treatment for type 2 diabetes, there’s an increasing acknowledgment of its potential as a supplementary approach.


The management of type 2 diabetes is not confined to medication alone.
Diet plays a paramount role, and incorporating magnesium-rich foods is a vital part of that strategy.
Specific foods known for their high magnesium content include leafy greens like spinach, whole grains such as brown rice, nuts like almonds, and seeds such as pumpkin seeds.
Even some fish, like mackerel, are rich in magnesium.
Lifestyle practices, such as regular exercise and stress management, also complement magnesium supplementation.
Exercise can enhance insulin sensitivity, while stress management is crucial as stress can interfere with magnesium’s effectiveness in the body.
Lastly, the integration of healthcare professionals cannot be overstated.
Dietitians, nutritionists, and medical doctors should work in concert to ensure that a patient’s magnesium intake, whether through diet or supplementation, is appropriately tailored to their individual needs and medical history.
Collaborative care not only optimizes magnesium’s potential benefits but also creates a comprehensive, patient-centered approach to managing type 2 diabetes.
While magnesium’s role in type 2 diabetes management is promising, it is not without challenges and controversies.
Implementing magnesium therapy can be complex due to individual variations in needs and responses.
What works for one person may not work for another, and an excessive intake can lead to adverse effects.
Additionally, there are differing opinions within the scientific community.
Some researchers caution that magnesium’s impact on glycemic control might be overstated or that other confounding factors might play a role.
This has led to some debate over how prominently magnesium should feature in standard diabetes care guidelines.
These complexities highlight areas that require further research.
Future studies should focus on pinpointing the optimal levels of magnesium intake for different populations and understanding the precise mechanisms by which magnesium interacts with insulin and glucose metabolism.
Only through rigorous and nuanced investigation can we fully unlock magnesium’s potential in diabetes care.


In the quest to manage and potentially prevent type 2 diabetes, magnesium has emerged as an essential player.
This blog has explored its multifaceted role in the body, from its effect on insulin sensitivity to its application through diet and supplementation.
We’ve examined real-life cases, clinical trials, and guidelines that substantiate magnesium’s promise, all while recognizing the existing challenges and controversies.
The importance of magnesium in type 2 diabetes management is becoming increasingly clear, but it is not a one-size-fits-all solution.
Therefore, a call to action for readers: Consider your individual needs and consult with healthcare professionals to tailor a magnesium-centric approach that suits you best.
As we look to the future, continuous research and a personalized, patient-centered approach will remain key.
The exploration of magnesium in diabetes care is an exciting frontier, one filled with potential and worthy of our continued attention and investigation.
Thank you for joining us on this exploration of magnesium’s vital role in the fight against type 2 diabetes.
Here’s to empowering ourselves with knowledge and taking proactive steps towards better health.
References:
Global Prevalence of Type 2 Diabetes:
Magnesium and Diabetes Relationship:
Magnesium Deficiency in Diabetics:
Clinical Trials and Real-World Evidence:
Dietary Sources and Supplementation:
Potential Risks and Balancing Minerals:
Guidelines and Recommendations:


In recent years, seed milks have gained popularity as a nutritious and eco-friendly alternative to dairy and other plant-based milks. Marketed as a healthy option, these beverages are often touted for their rich nutrient profiles and sustainability. However, a closer look reveals that not all seed milks are created equal. Many contain hidden ingredients and […]


NOTICE TO THE PUBLIC! A vast array of products seen in American grocery stores are notably absent on European shelves. This is not due to a lack of international trade but rather stringent food safety regulations in the European Union. Many popular American foods are banned in Europe due to concerns about health risks and […]


Did you know that there lurks an invisible ingredient in meat that has been raising health concerns —It is called meat glue- scientifically known as transglutaminase? Transglutaminase is an enzyme used to bind pieces of meat together to create larger, more uniform cuts that creates a seamless appearance. According to the American Meat Institute, it […]